On Monday I gave a double lecture. The first part was about cardiovascular embryology, and the heart in particular, and the second part was about the changes to the cardiovascular system that occur with birth and the baby’s first breath. The second part is normally delivered by Dr Geraint Morris, a consultant paediatrician and neonatologist far more able to talk about these things and their clinical relevance and examples than me, but unfortunately a scheduling snafu meant he was unable to be there.
I think Rhi and I have written 4 short chapters about the development of blood vessels and the heart, but I won’t try to reproduce that here. Probably the most relevant and important parts for medical students to understand are how the heart is formed and split into chambers, and how well oxygenated blood from the placenta bypasses the foetal lungs and gets to the developing brain instead.
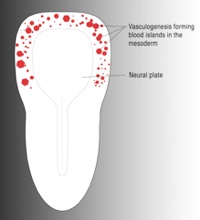
I talked about the differences between vasculogenesis and angiogenesis, the former being important in the early embryo (from around day 19) and the latter occurring during development, repair, in the endometrium during the menstrual cycle, and in tumour growth. Anti-angiogenic drugs have been developed to target the growth of tumours.
Vasculogenesis describes the appearance of new blood cells and blood vessels as if by magic; from out of thin air. Of course what really happens is that mesoderm cells differentiate into a “haemangioblast”, or if you prefer, into haemoblasts and angioblasts. Angioblasts will form new blood vessels.
Angiogenesis is defined as the formation of new blood vessels from existing ones. The term intussusception is often used here, and describes the splitting of a blood vessels into two.
So if we’re going to talk about how the heart develops, we first need to bring together these little pockets of new blood vessels that are forming in a horseshoe shape around the head end of the early, flat embryo.
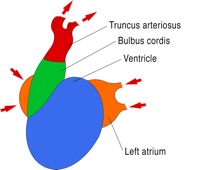
The embryo folds laterally and along its length, rolling up to form the body wall and bringing some of those early blood cysts together to form the early heart tube, which lies a little inferior to the head. At an early stage this simple tube receives blood from 3 pairs of veins at a sinus venosus, squeezes it through an early atrium, ventricle, bulbus cordis and out through a truncus arteriosus into the early arteries of the neck and into paired dorsal aortae.
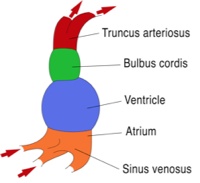
The next phase must include splitting the heart up into the four chambers that we recognise in the adult heart, and the processes that do this pretty much all run at the same time. We’ll talk about them separately though, and will start with the splitting of the atrium from the ventricle.
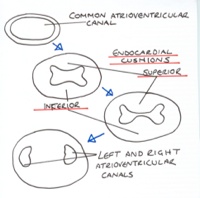
The heart tube folds to bring the atrium posterior (dorsal) to the ventricle. At the junction between the atrium and ventricle the endocardium in the walls starts to plump up, and the atrioventricular canal starts to narrow. These “endocardial cushions” thicken, and the ventral and dorsal cushions grow towards each other and meet, splitting the atrioventricular canal into two.
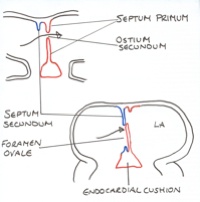
The single atrium is split into two at the same time but in a slightly more complex manner, and this may be a story you’re aware of. Failure of this process can leave an atrial septal defect, which is different to a patent foramen ovale. You’ve probably seen the fossa ovalis in the adult heart. So what normally happens?
From the roof of the single atrium a wedge of endocardium begins to grow down towards the endocardial cushions. Think of it as a thin, curved, extending wedge. This is the septum primum (the first fence). It splits the atrium into two atria, but before it meets the endocardial cushions and completes this, a hole forms high up in the septum primum. This is the ostium primum (the first hole). In this way the left atrium remains connected to the right atrium.
Next, a second, curved wedge of endocardium descends from the roof of the right atrium, beside the septum primum. This is the septum secundum. This wedge of endocardium will never quite reach the endocardial cushions. The hole that remains beneath it is called the septum secundum.
In the foetus pressure within the right atrium is higher than in the left atrium. The blood entering the right atrium is returning from the systemic circulation and from the placenta, whereas blood entering the left atrium is returning from the developing lungs. At this time resistance to blood flow through the lungs is high.
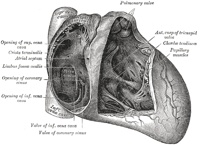
The well-oxygenated blood entering the right atrium of the heart (from the placenta) rushes across into the left atrium through the foramen ovale. The foramen ovale has formed from the flap of the septum primum flapping against the septum secundum that acts as the doorstop. So blood in the right atrium pushes open the flap of the foramen ovale. The eustachian valve of the inferior vena cava (labelled as “valve of inf. vena cava in the Gray’s Anatomy illustration below) entering the right atrium helps direct the flow of blood through the foramen ovale. By avoiding the lungs, well-oxygenated blood can pass through the left atrium, left ventricle, and out of the heart and up into the carotid arteries to get to the developing brain with only a small loss in oxygen and nutrient content.
At birth, when the lungs begin to work, the resistance to blood flow through the lungs drops. Blood flows through the lungs and back into the left atrium. The blood pressure in the left atrium is then higher than in the right atrium, and the flap (septum primum) of the foramen ovale is pushed closed against the septum secundum. From this point onwards blood will no longer normally flow from the right atrium to the left atrium through this valve, although changes in thoracic pressure with coughing or sneezing may cause this. A little while after birth the edges of the foramen ovale become sealed and fixed, and it becomes the fossa ovalis.
The next time you look into the right atrium of a heart model or prosection have a look for the fossa ovalis and the curve of the eustachian valve.
The single ventricle is split into two ventricles by two structures. The myocardium from the floor of the ventricle grows up towards the endocardial cushions, starting to split the chamber into left and right ventricles. It never quite reaches the endocardial cushions though. This is the muscular interventricular septum.
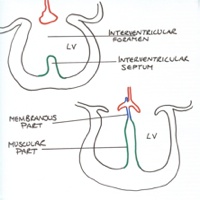
The conotruncal outflow tract (it has conus arteriosus and truncus arteriosus sections) is the single outflow tract of the early heart. Rather like the endocardial cushions, two ridges of endocardium grow along the length of the conotruncal tube, within it, opposite one another, but in a spiral (or helical) manner. They grow towards each other, meet as the conotruncal septum, and split the conotruncal outflow tract into the two great vessels: the aorta and pulmonary trunk (or artery).
The conotruncal septum also meets with the muscular interventricular septum, finishing the splitting of the ventricles into left and right and connecting the aorta to the left ventricle and the pulmonary trunk to the right ventricle. This is the membranous interventricular septum. If this all doesn’t come together quite right there maybe an interventricular defect, or the aorta and pulmonary trunk may be connected to the wrong sides of the heart.
By the way, that spiralling of the conotruncal septum can be seen in the adult heart, as the aorta and pulmonary trunk spiral around each other.

There’s a little shortcut vessel in the foetus, between the pulmonary trunk and the aorta, called the ductus arteriosus. This is another route by which blood can avoid going through the lungs, and blood in the pulmonary trunk will pass through the ductus arteriosus and into the aorta, rather than into the lungs.
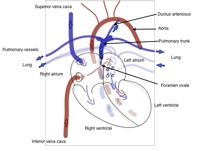
With birth the constricted blood vessels of the lungs dilate, reducing resistance to flow. Blood passing through the pulmonary circulation becomes rich in oxygen, and passes into the left side of the heart and the aorta. Backflow of this oxygen-rich blood into the ductus arteriosus from the aorta triggers the smooth muscle of the ductus arteriosus to constrict (along with other, more complex mechanisms). It closes up, and in the adult this is called the ligamentum arteriosum.
Similarly, the umbilical vessels also constrict, pushing blood back into the foetus, and become ligamentous strands in the adult.
You can review all this with some of the links below. The YouTube video I showed in the lecture. Dr Morris couldn’t teach this year so I covered his lecture, and there is a podcast below covering similar stuff.
Links:
The YouTube video of heart development
Heart development podcast (Webster, de Wreede)
Changes to circulation at birth podcast, with Dr Geraint Morris (Webster, de Wreede)
Stages of vascular development – mouse embryo
Patent ductus arteriosus – PubMed Health
Persistent pulmonary hypertension of the newborn – Medscape Reference
Gray’s Anatomy heart illustration, Wikimedia Commons source